Overview
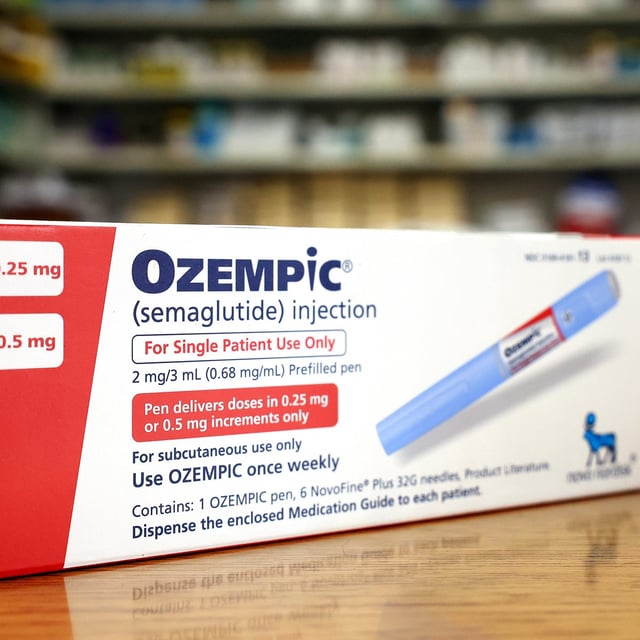
- The Centers for Medicare & Medicaid Services plans a five-year experiment run by its innovation lab to allow voluntary coverage of Ozempic, Wegovy, Mounjaro and Zepbound for weight management
- The pilot will begin in April 2026 for state Medicaid programs and roll out in January 2027 for Medicare Part D plans
- Annual treatment costs of $5,000 to $7,000 per patient have raised questions about long-term affordability for both federal and state budgets
- The Congressional Budget Office estimates that obesity coverage of GLP-1 drugs could cost Medicare about $35 billion from 2026 through 2034
- Thirteen state Medicaid programs already cover GLP-1s for obesity, and the pilot will gauge participation levels, patient outcomes and potential budget impacts