Overview
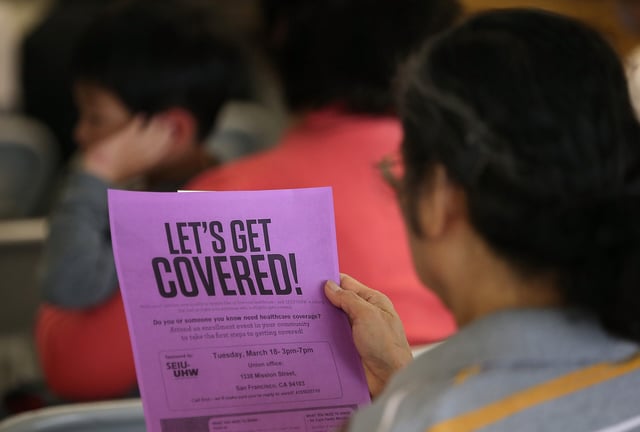
- The 2025 federal budget law cuts $1 trillion from Medicaid funding over 10 years and ends Affordable Care Act marketplace subsidies after December, risking a 66% average premium hike in Covered California plans.
- Beginning December 2026, adults 19 to 64 must log 80 monthly hours of community engagement or face Medi-Cal disenrollment, with co-payments up to $35 per visit set to start in October 2028.
- State estimates project a $28.4 billion federal funding loss and 3.4 million Californians losing coverage over the next decade, including 1.4 million due to new work requirements.
- Providers warn that an influx of uninsured patients, tighter income verifications and reduced federal reimbursements could force service cuts, staff layoffs or hospital closures.
- A federal judge has temporarily blocked the immediate ban on Planned Parenthood Medi-Cal payments as CHIP eligibility for immigrant children is narrowed to legal permanent residents.