Overview
- The Center for Medicare and Medicaid Innovation will oversee a five-year pilot enabling state Medicaid programs and Medicare Part D plans to opt in to GLP-1 weight-loss drug coverage for “weight management.”
- Coverage can begin in April 2026 for Medicaid and January 2027 for Medicare, reversing earlier decisions that excluded the drugs and replacing a Biden-era expansion proposal.
- Plans choosing to participate must offer patients diet and exercise coaching alongside medication to support metabolic health and maximize treatment benefits.
- Congress’s budget office estimates extending GLP-1 coverage could cost Medicare about $35 billion from 2026 through 2034, highlighting concerns over fiscal sustainability.
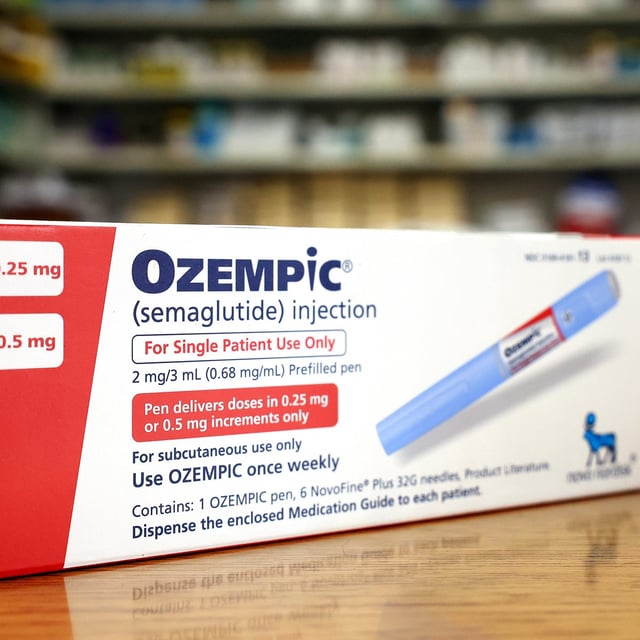
- Annual treatment expenses range from $5,000 to $7,000 per patient, and state participation remains uncertain despite 13 Medicaid programs already covering medications such as Ozempic, Wegovy, Mounjaro and Zepbound.