Overview
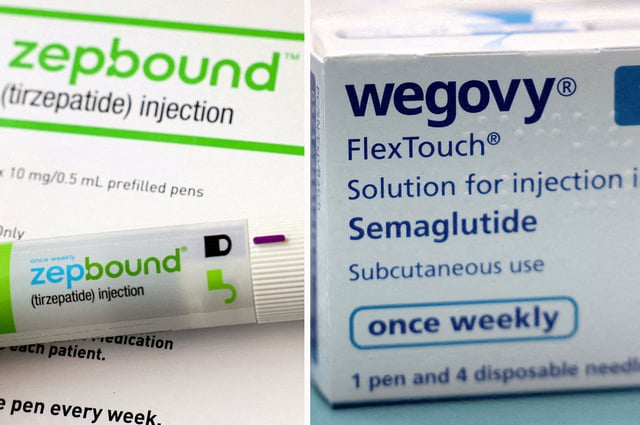
- Blue Cross Blue Shield of Massachusetts has announced it will no longer cover GLP-1 drugs like Ozempic and Wegovy, citing financial losses from soaring demand.
- Point32Health, the state’s second-largest insurer, will continue covering GLP-1 medications, positioning itself competitively despite rising costs.
- The Trump administration recently rescinded a Biden-era proposal that would have mandated Medicaid coverage of GLP-1s for obesity, leaving coverage decisions to individual states.
- A new Aon study shows that GLP-1 treatments can reduce overall healthcare costs by 7% within two years, driven by significant decreases in cardiovascular events and related conditions.
- Medicare continues to exclude GLP-1 drugs for weight loss but covers them for cardiovascular risk reduction, reflecting ongoing policy limitations on broader access.